A percutaneous coronary intervention procedure is a common procedure performed to open up arteries that are clogged or narrowed due to fatty deposits. The procedure can also be referred to as a coronary angioplasty, a balloon angioplasty, or more commonly as a stent.
The term stent refers to the small mesh tube made of metal, which acts like scaffolding that supports the artery, keeping it open and improving blood flow.
“Percutaneous” simply means “through the skin”, because a catheter is inserted through the skin and into the artery.
A percutaneous coronary intervention is most commonly performed as an elective procedure, but it can also be done as an emergency procedure following a heart attack.
This article explains what happens during a percutaneous coronary intervention (PCI) procedure and the potential risks and complications of the procedure. It also outlines what to expect before, during and after a PCI.
Why a percutaneous coronary intervention procedure is needed
A percutaneous coronary intervention is a minimally invasive surgical procedure performed by an interventional cardiologist under sedation and local anaesthetic to help restore blood flow to the heart due to blocked arteries.
This will improve the symptoms experienced by patients with partially blocked arteries – such as chest pain (angina) and/or shortness of breath – and help to reduce the risk of a heart attack.
Atherosclerosis is a condition caused by fatty deposits that build up in the arteries leading to the heart. These fatty deposits, or plaque, clog and narrow the coronary arteries and reduce blood flow to the heart. This puts pressure on the heart and can cause chest pain (angina) or a heart attack (myocardial infarction).
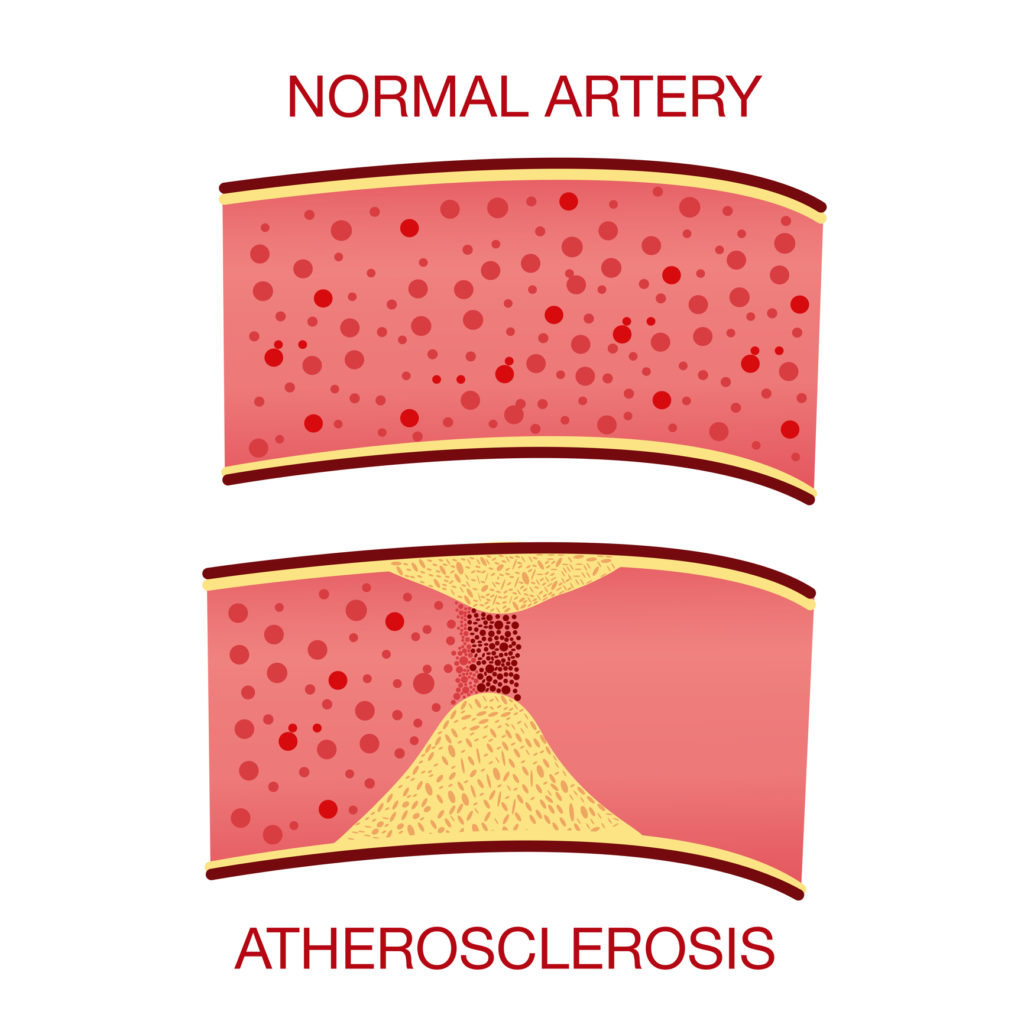
Above: Atherosclerosis is the buildup of fatty deposits in the arteries leading to the heart.
“A percutaneous coronary intervention will improve blood flow to the heart, helping to prevent angina or a potential heart attack”, says Doctor Mark Pitney, the Medical Director of Sutherland Heart Clinic.
“If you’ve had angina or a heart attack, a percutaneous coronary intervention is a life-saving procedure that opens up the arteries. It’s a very common procedure at Sutherland Heart Clinic to treat angina or heart attacks to allow the heart to function at its best.”
More than 1,500 PCI procedures have been performed every year at Sutherland Heart Clinic since it opened in 2006. Research shows that clinics that perform high numbers of procedures every year have fewer adverse events.
Our highly skilled team of surgeons, anaesthetists and nurses have extensive experience caring for patients undergoing this type of procedure.
Percutaneous coronary intervention: potential risks and complications
A percutaneous coronary intervention is generally a low risk procedure that’s performed regularly at Sutherland Heart Clinic.
However, as with any medical procedure, there is a small risk of complications. You’ll be given information about potential risks and complications by your doctor before your procedure.
It is common to have some bruising and swelling at the site where the catheter is inserted.
While the overall risk of complication is low, more serious risks include:
- an allergic reaction to the X-ray dye
- infection
- bleeding at the insertion site
- pain
- blood clots
- re-narrowing of the artery
- abnormal heart rhythms (arrhythmias)
- heart attack
- coronary artery damage
- stroke
- damage to the kidneys
After the procedure, there is a small risk that blood clots may form within the stent, which can cause a heart attack. You will be prescribed blood-thinning medication to take after the procedure to reduce the risk of a clot forming. Your doctor will talk to you about what medication you’ll need to take, and for how long.
If you have any concerns about the procedure, it’s important to discuss these with your doctor before your procedure.
Managing your medications before and after an angioplasty procedure
Some medications may need to be stopped a few days before having a percutaneous coronary intervention (also known as an angioplasty), especially if you’re taking medication such as Warfarin, Lasix or insulin.
Your doctor will talk to you about your medications in advance of your procedure. It’s important not to stop or change any medications until you’ve discussed this with your doctor first.
If you’re taking Warfarin, your doctor will tell you whether you need to stop taking it three days before your procedure. You may need to take an alternative anticoagulant (blood thinner) during this time.
“Keep taking your medication until you’ve discussed it with your doctor. They will tell you if and when to stop taking any medication,” Dr Pitney said. “They will also let you know when you can start taking your medication again.”
Your doctor will also talk to you about what medication you’ll need to take after a percutaneous coronary intervention. Generally, having a stent means you’ll need to take blood-thinning medication long-term to reduce the risk of developing a blood clot.
If you have any questions about your medication, ask your doctor or phone your cardiology clinic.
Getting ready for your PCI procedure
In the weeks leading up to your procedure, you’ll need to have some blood tests and plan your going home arrangements.
On the day of the procedure, you’ll need to start fasting in the morning. At Sutherland Heart Clinic, we ask our patients to stop eating solid food six hours before their admission. You can have clear fluids at that time, but no cloudy or milky drinks. Two hours beforehand, you’ll have to stop drinking any fluids, including water.
Your clinic will give you more detailed instructions before admission. You can also read more about fasting before your visit. If you have any questions, contact your clinic beforehand.
What happens during a PCI procedure?
The percutaneous coronary intervention will be done in a cardiac catheter laboratory, which looks like an operating room. The procedure takes about 90 minutes, depending on the state of your coronary artery or arteries.
Prior to your procedure, you’ll be asked to change into a hospital gown. If you wear glasses and/or hearing aids, most doctors allow you to wear them during your procedure.

Above: Our expert team will look after you at every stage of the procedure.
You will then be asked to lie down on a narrow procedure table. Your cardiologist, anaesthetist and other experienced cardiology nursing staff will be there to look after you throughout the procedure.
The procedure will be done under either a local or a general anaesthetic. Your surgeon and anaesthetist will talk to you about what type of anaesthetic is best suited to you based on your particular health needs.
Your doctor will let you know where they will insert the catheter. This is generally either in the femoral artery in the groin or the brachial artery in the arm. If it’s inserted via your groin, the theatre staff may shave around that area first, if this is needed.
Your anaesthetist will then insert a drip to maintain your fluids, and you’ll be offered sedation to help you relax. You will also be given a local anaesthetic at the site where the catheter (a thin, flexible hollow tube) will be inserted.
A guide wire is then inserted into the artery. An X-ray dye known as “liquid contrast” is injected through the catheter, which can sometimes cause a warm sensation. The dye enables X-ray images of the heart to be taken so your cardiologist can see where the artery has narrowed.
A small balloon catheter is then inserted via the insertion site. This is why percutaneous coronary intervention is sometimes called a “balloon angioplasty”.
The balloon is inflated and deflated several times to open the artery. Then the stent is implanted into the artery, via the catheter. You may feel some discomfort when the balloon is inflated, because the heart will be momentarily deprived of oxygen.
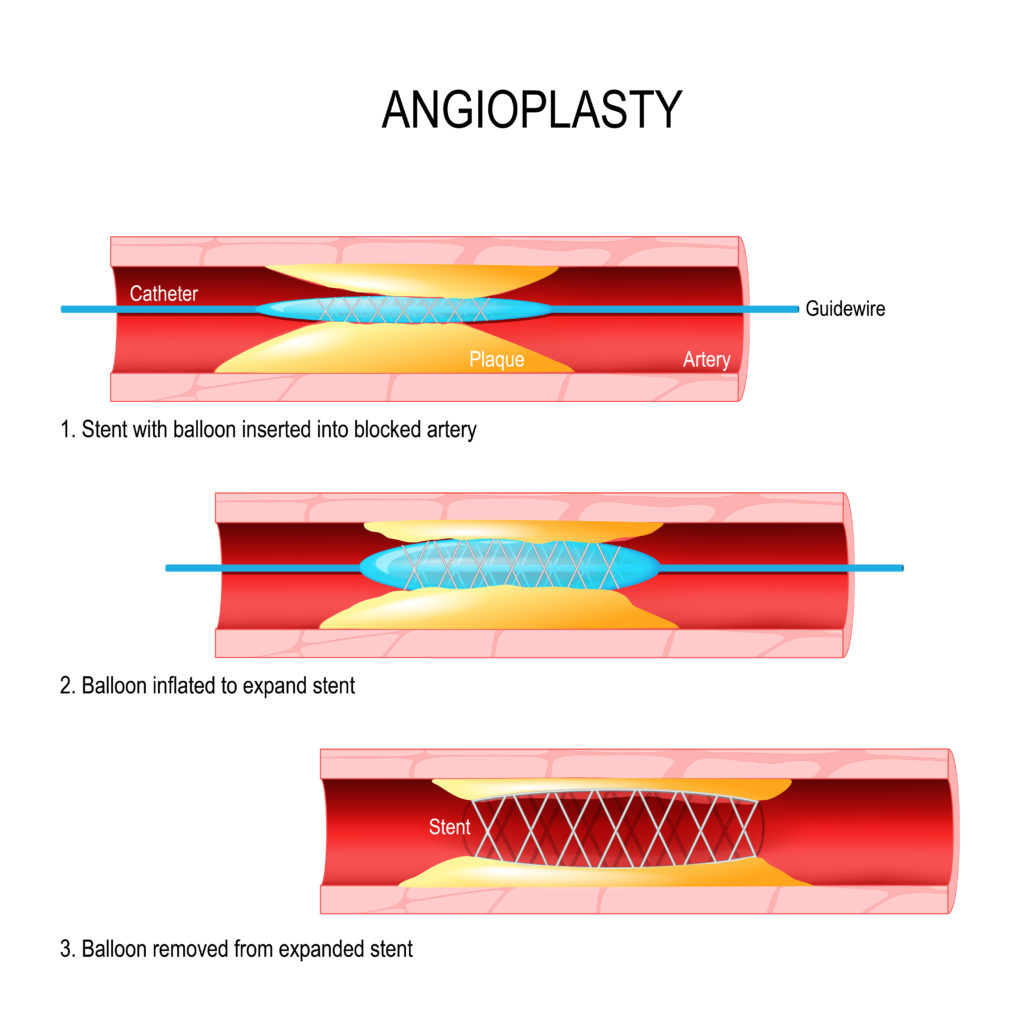
Above: An illustrative explanation of the inflation of the balloon catheter and insertion of the stent.
“Patients sometimes experience angina at this stage of the procedure, but this is only temporary and will resolve as soon as the balloon is deflated,” Dr Pitney says.
“The medical team will be there to take care of you and respond to any pain you may experience.”
The stent is then put into the artery and expanded using the balloon. Unlike the balloon, which is only used during the PCI procedure, the stent remains inside the artery permanently.
Once the stent is in place, the balloon is inflated and the catheter is removed.
What should I expect immediately after the PCI procedure?
After your procedure, you’ll be transferred to the recovery room. You’ll need to lie flat for about four hours and your blood pressure and wound will be closely monitored.
You may experience some discomfort in your chest and, if this is the case, you’ll be offered analgesia to keep you comfortable. You’ll also be encouraged to drink lots of fluids to help flush out the contrast dye.
Sometimes patients stay in hospital overnight following a percutaneous coronary intervention and are discharged home the following morning. This will depend on the time of your procedure, and what your doctor considers is best for you.

Above: Dr Mark Pitney discussing the results of a procedure with a patient
Recovering from a percutaneous coronary intervention procedure
As you will have had sedation for your procedure, it’s a good idea to avoid drinking alcohol or making any major decisions until the effects have completely worn off.
You won’t be able to drive (or fly) for 24 hours afterwards, so you’ll need to arrange for someone to take you home. If you live by yourself, we suggest asking someone to stay with you for the first night after the procedure, so someone is close by in case you need any assistance or support.
When you’re recovering at home, keep an eye out for any bleeding at the site where the catheter was inserted. It’s normal to have some pain and bruising at the puncture site, but call the clinic if you are concerned.
Contact your angiogram clinic if you experience any:
- chest pain or tightness
- fever
- swelling or bleeding where the catheter was inserted
- weakness of numbness in the limb where the catheter was inserted
Call an ambulance straight away if you experience:
- significant bleeding or swelling of the wound
- chest pain or tightness that increases or is severe
If you have any general questions or concerns about your recovery, contact your doctor’s rooms or the clinic for advice.
About Sutherland Heart Clinic
Sutherland Heart Clinic is a major interventional cardiology hospital co-located with Sutherland Hospital at Caringbah in Sydney’s southern suburbs. The clinic offers a wide range of procedures including diagnostic studies, angioplasty procedures (with stents) and pacemaker procedures.
Learn more about our clinic, cardiology procedures, and what to expect if you’ll be visiting us for a procedure.
Read more:
Coronary angiogram: Our complete guide
Day of the procedure
Before your visit
After your visit
Patient privacy and rights


Recent Comments